What is Mitochondrial Disease?
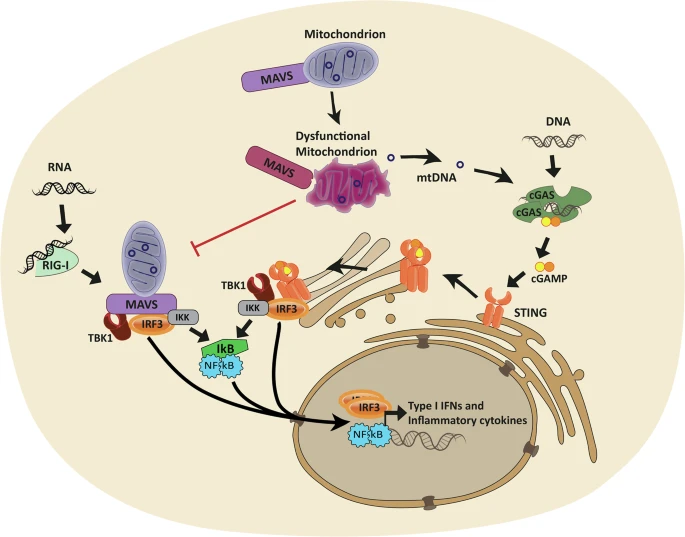
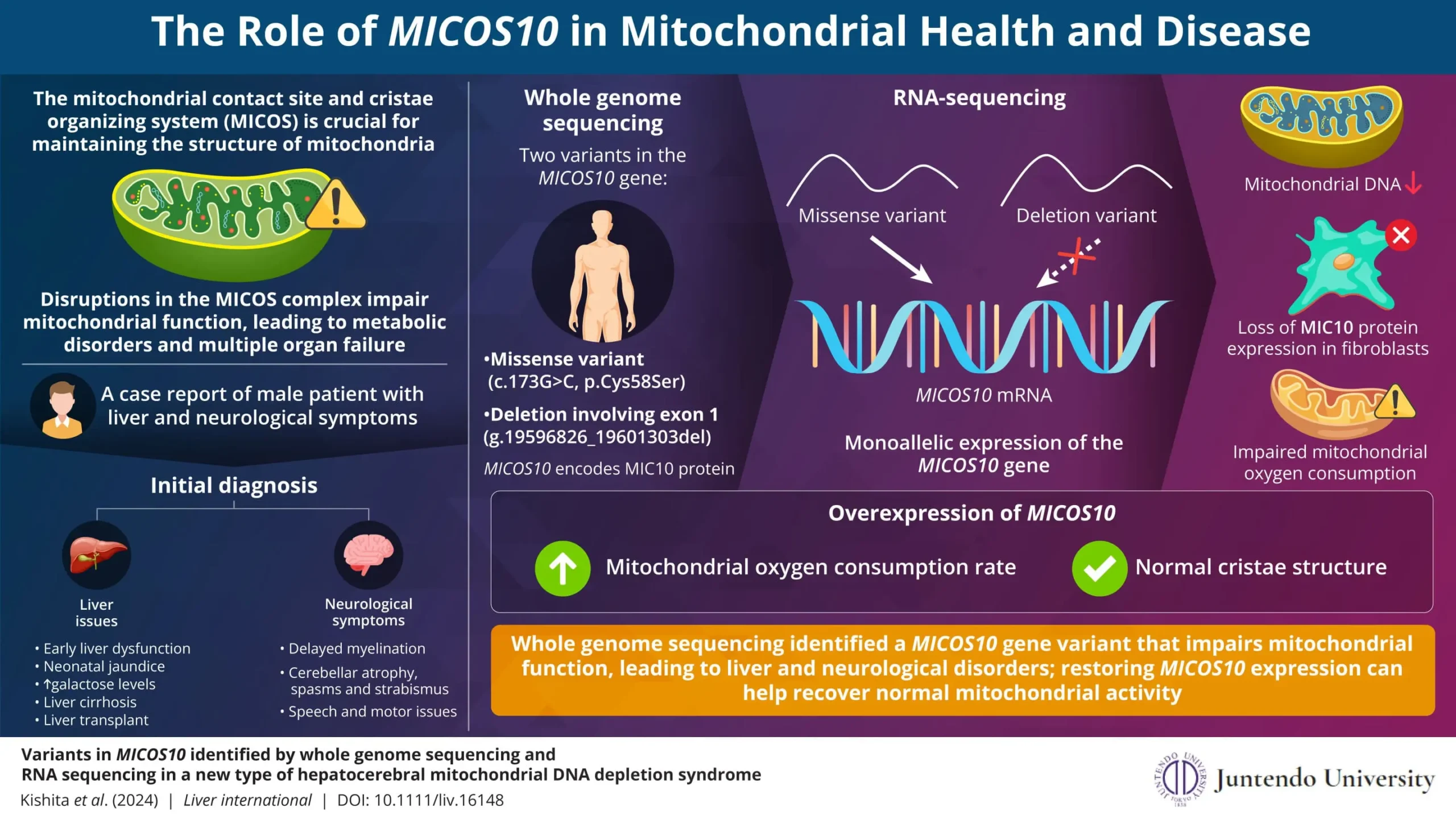
Mitochondrial disease occurs when the mitochondria in the body’s cells can no longer produce adequate energy. This can lead to the failure of individual cells and, eventually, the malfunction of entire organ systems. Given that mitochondria are involved in nearly every bodily function, this disease can affect multiple organs and systems simultaneously, making it difficult to diagnose and treat.
The condition is typically inherited and can be caused by mutations in either the mitochondrial DNA (mtDNA) or the nuclear DNA (nDNA) that controls mitochondrial function. There are also environmental factors, like toxins, that can damage mitochondria and contribute to the disease. The severity and specific symptoms of mitochondrial disease vary significantly from one individual to another, making each case unique.
The Importance of Mitochondria in the Human Body
Mitochondria are tiny but essential structures within almost every cell of the human body. Known as the “powerhouses” of the cell, they are responsible for producing up to 90% of the energy the body needs to sustain life and support essential functions. From your brain to your muscles, every organ relies on mitochondria for the energy required to perform daily tasks.
In a healthy body, mitochondria convert the food we eat and the oxygen we breathe into adenosine triphosphate (ATP), the energy molecule that fuels everything from muscle contraction to nerve transmission. However, when mitochondria malfunction due to genetic mutations or environmental damage, this process can be severely disrupted. The result is mitochondrial disease, a condition that affects cellular energy production and can lead to multi-organ failure.
Every 30 minutes, a child is born who will develop mitochondrial disease by the time they reach 10 years old.
Symptoms of Mitochondrial Disease
The disease can affect any part of the body, but it tends to hit organs that require a lot of energy the hardest. This includes the heart, brain, muscles, and nerves, but other organs such as the liver, pancreas, and kidneys can also be affected.